“Digital Eyes” for Clinicians: AI Becomes an Official Tool in Preventive Health Screenings
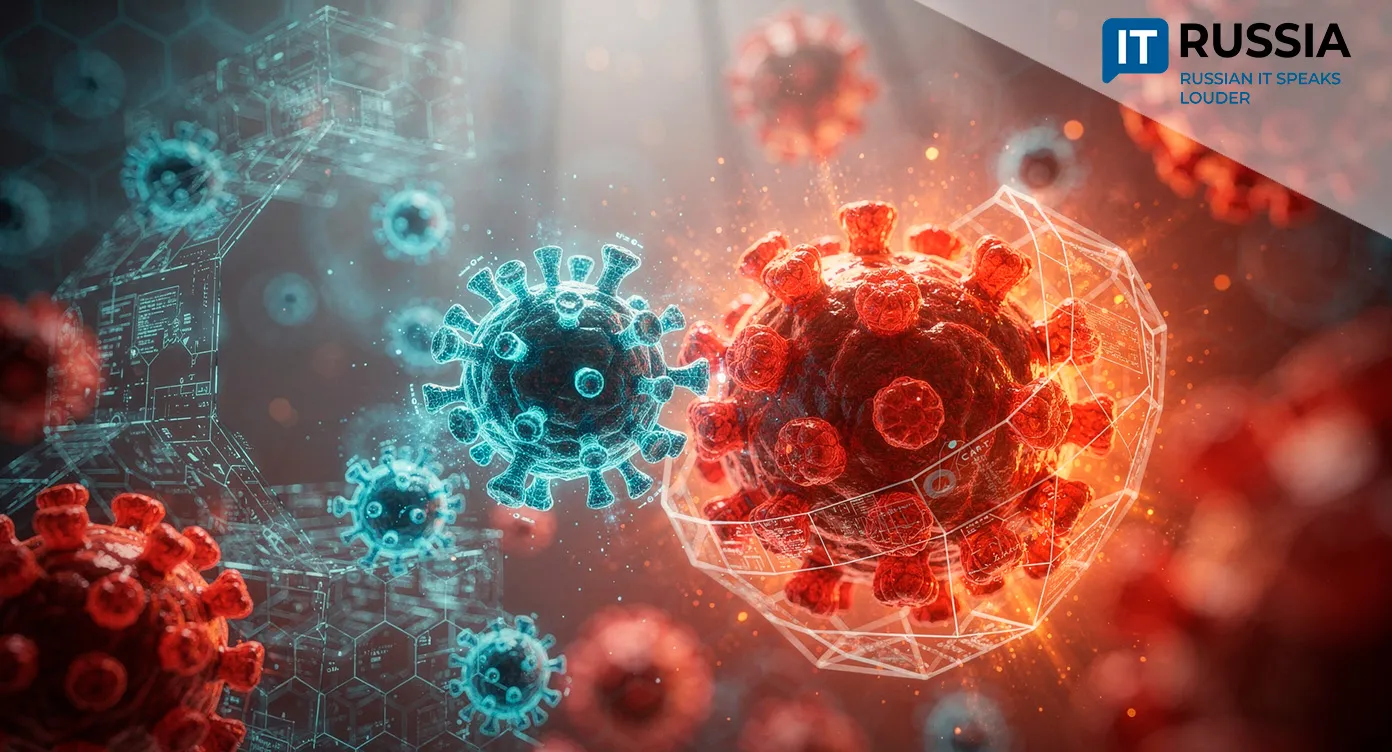
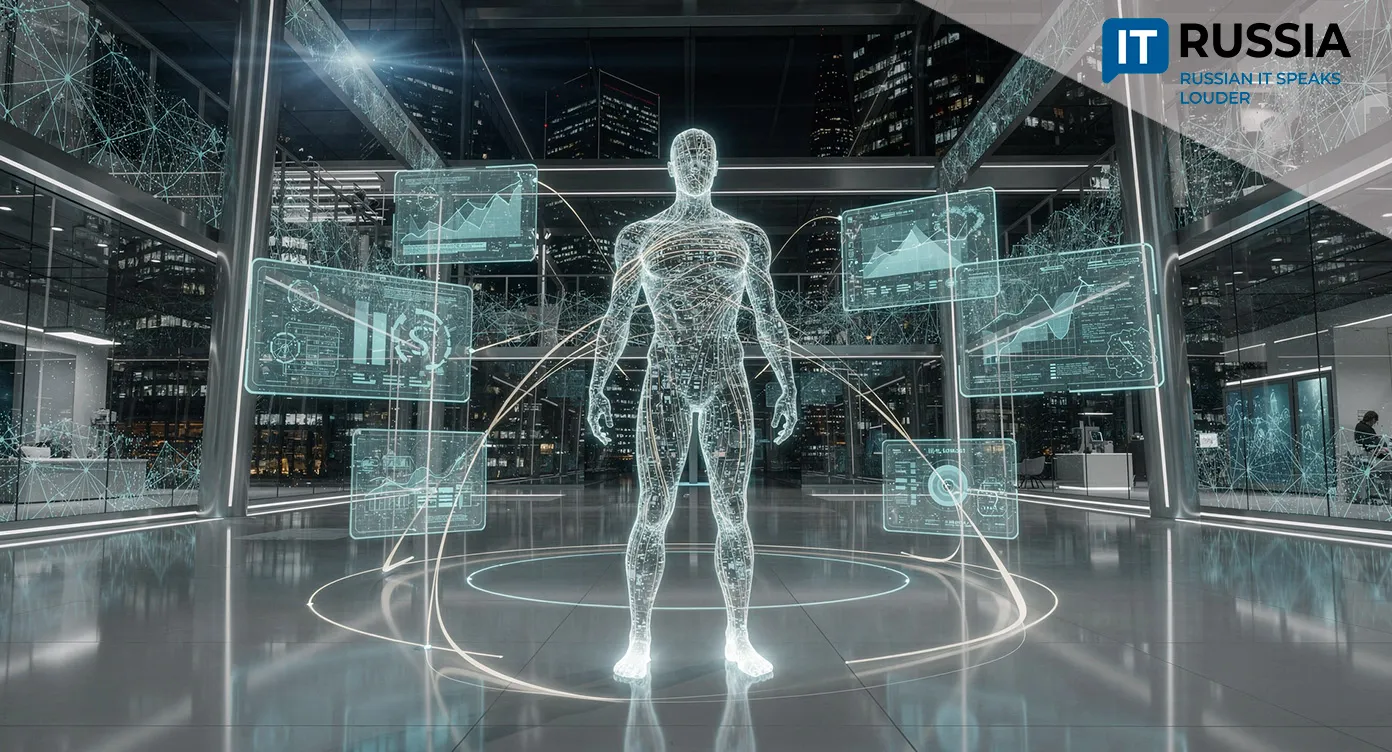
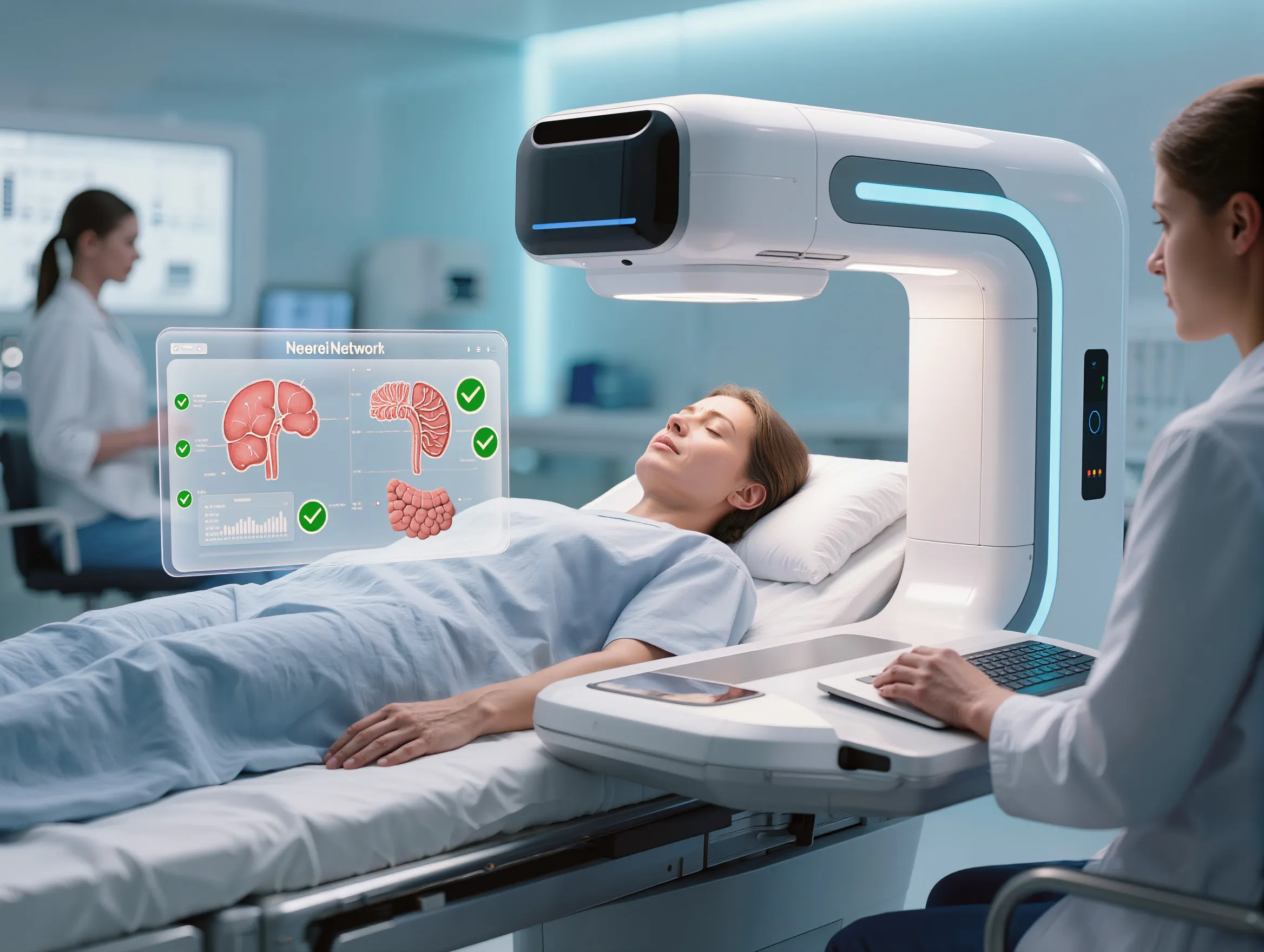
Starting in 2026, artificial intelligence in Russia will begin assisting physicians at scale in analyzing patient imaging as part of annual preventive health screenings. Funding for this software has now been formally included in the national compulsory health insurance framework, with algorithms set to review mammograms, lung CT scans, ECGs, and other diagnostic studies.

AI Reaches the Regions
Russia has taken a step that will soon affect millions of people, while remaining almost invisible to them in everyday life. From 2026 onward, AI systems will assist physicians in interpreting medical images – including mammograms, chest X-rays, CT scans, colonoscopy images, and even cardiograms.
According to Russia’s Minister of Health Mikhail Murashko, funding for this software has been officially incorporated into reimbursement standards for preventive checkups and population-wide health screenings. In practical terms, AI becomes a new digital instrument in the hands of primary care doctors and radiologists, paid for through the compulsory health insurance system.
This is not the first experiment with intelligent algorithms in outpatient clinics. Over the past five years, various image-analysis systems, particularly those used for COVID-19 diagnostics, were piloted in several regions and individual medical centers. What changes now is the scale. The technology is being rolled out systematically as part of the national screening program. AI tools will operate not only in major research hospitals in Moscow or St. Petersburg, but also in routine urban clinics and regional hospitals across the country. An AI assistant reviewing thousands of images shifts from being an innovation to a standard medical procedure available under a public insurance policy.
What Will Change for Patients
The main value of this shift lies in its direct impact on individuals. For patients, the changes fall into three key areas.

First, speed will increase. An algorithm can analyze an image in seconds and flag potentially suspicious areas for the physician – possible tumors, opacities, or tissue changes. This does not replace the specialist, but helps them focus more quickly on areas of concern, reducing the time needed for initial review.
Second, prevention will become more effective. AI does not tire or lose concentration. It can act as an additional, highly attentive “set of eyes,” reducing the risk of missing early signs of disease at the stage when treatment is most effective. This is particularly important in mass screening programs, where clinicians work under heavy workloads.
Third, geographic barriers are reduced. Dedicated funding has also been allocated for integrating these systems into telemedicine workflows. As a result, expert evaluation of a complex image from a district hospital can be obtained almost instantly. This is a direct path toward narrowing the gap in care quality between major cities and remote areas.
Data, Experience, and New Standards
For the healthcare system, this decision triggers several important processes. The vast volume of data generated through millions of examinations will become the foundation for training and refining the algorithms themselves. AI quality improves as the volume and diversity of data grow, allowing the system to evolve continuously.
At the same time, large-scale deployment creates invaluable practical experience. Russian developers and clinicians will gain unique insight into how digital tools can be integrated into real clinical workflows, how staff should be trained, and how the effectiveness of such solutions can be assessed not in laboratory conditions but in everyday outpatient practice. This experience will form the basis for the next generation of more sophisticated medical AI systems.
Equally important is the role of the state as a customer. By embedding AI into a nationwide program, public authorities begin to set clear requirements and standards for these technologies. This, in turn, creates a regulated environment for the growth of an entire medical AI industry.
Looking Beyond Russia
Russia’s experience with the large-scale, systematic deployment of AI in a state-run preventive care program is of global interest. Many countries are experimenting with similar technologies, but few have the ability to test them across a national healthcare system with such broad population coverage.
If implemented successfully, the project opens opportunities beyond the domestic market. Proven solutions, their deployment methodologies, and the accumulated datasets could become attractive to other countries facing similar challenges – rising healthcare workloads, shortages of specialized physicians in regional areas, and the need to lower the cost of preventive care. Russian health IT companies that have gained experience working under large public contracts would then have a strong case for entering international medtech markets.

A Future That Has Already Begun
Introducing AI into preventive health screenings marks the start of a long journey. Over the next one to two years, significant effort will be required to select and fine-tune algorithms, train physicians, and adjust clinical workflows. The main challenge will not be the technology itself, but how seamlessly it is embedded into physicians’ daily work so that AI becomes a genuine assistant rather than an additional bureaucratic burden.
Even so, it is already clear that artificial intelligence is no longer an exotic concept in Russian healthcare. It is becoming part of everyday medical infrastructure. Its ultimate goal is to make disease prevention faster, more accurate, and more accessible for everyone. The fact that this shift has now received official status and funding is perhaps the strongest confirmation that the process is firmly underway.