A Digital Pathologist: How Russian AI Learned to Save Lives Before Disease Begins
Russian scientists and developers have created an artificial intelligence system capable of detecting precancerous conditions of the stomach with 96% accuracy. The system analyzes tissue samples many times faster than a human specialist and promises to reshape early diagnostics not only in Russia, but globally.
Early Diagnosis Means Lives Saved
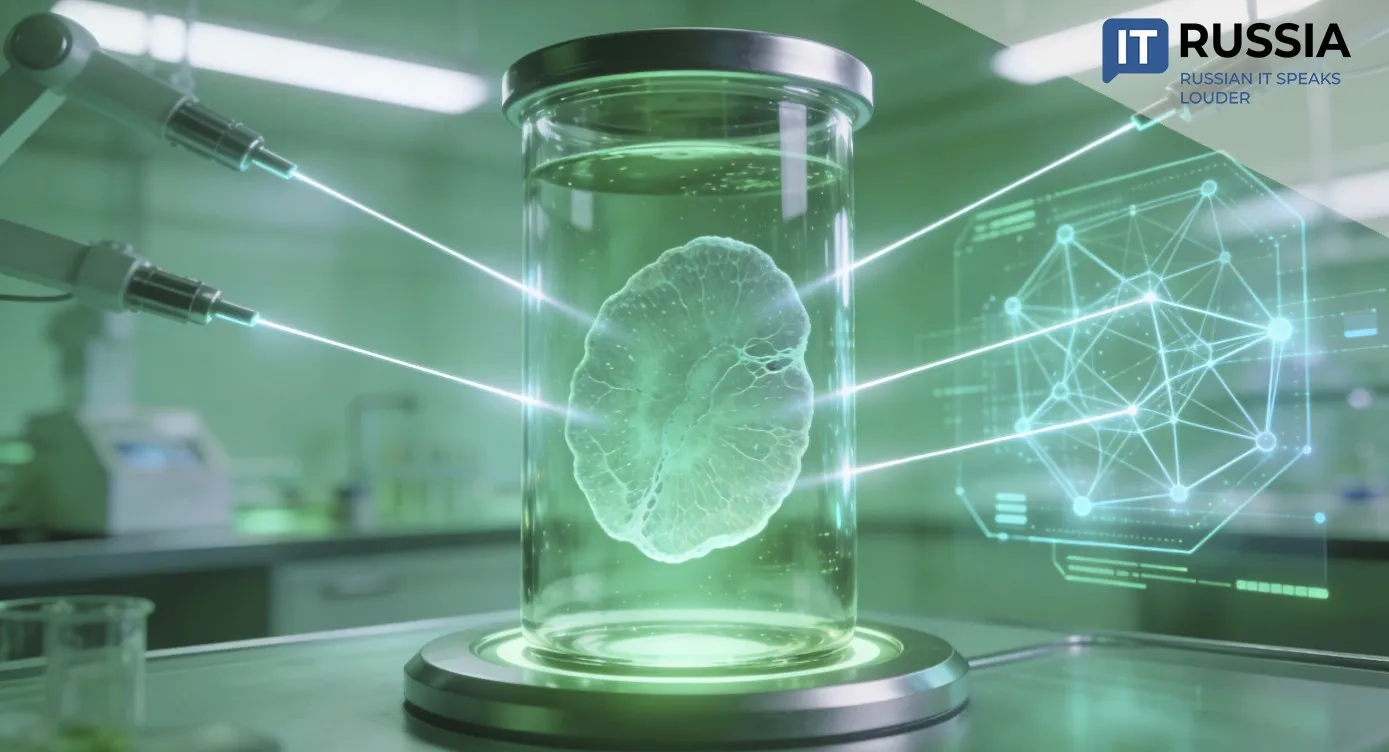
An event whose significance goes far beyond academic research has taken place in the laboratories of Sechenov University. Scientists and engineers, working in collaboration with specialists from Beeline Big Data & AI, have unveiled an AI system capable of diagnosing atrophic gastritis from histological sections of gastric tissue with an unprecedented 96% accuracy. The algorithm analyzes images, highlights pathological areas, and assesses the extent of tissue damage. The system is built on more than 5,500 carefully annotated medical images, a full year of machine learning, and deep expertise at the intersection of medicine and data science.
Atrophic gastritis is not merely inflammation. It is a process in which the stomach’s mucosal lining thins and functional cells are replaced by intestinal-type cells. The disease can progress silently for years, yet it is the primary and direct precursor to gastric cancer, one of the most aggressive oncological conditions. This long asymptomatic phase is where the greatest danger lies.

Traditional diagnostics represent a lengthy pathway for patients: endoscopy, biopsy sampling, and painstaking work by a pathologist examining microscopic tissue sections. The process demands extreme concentration, takes anywhere from 15 minutes to several hours per case, and final results are often delivered days later. Even among experienced specialists, assessments of the same sample can vary by 5% to 15%.
The new algorithm functions as a tireless, hyper-attentive assistant. It dramatically reduces analysis time, standardizes conclusions, and directs physicians’ attention to the most critical tissue areas. Cutting diagnostic turnaround times from four to seven days down to two or three is not a matter of administrative efficiency. In oncology, every day matters, and faster decisions translate directly into lives saved.

A Russian Approach: Combining Scientific Depth With Data
The project’s success is rooted in a distinctive competitive advantage: the ability to combine a world-class fundamental scientific school with advanced industrial IT capabilities. Sechenov University represents the country’s largest medical research and education cluster, with access to vast archives of real clinical data. The Beeline Big Data & AI team contributed expertise in large-scale data processing, machine learning, and industrial deployment of complex algorithms.
The result is not a generic “AI for everything,” but a highly specialized, deeply trained tool designed for a specific, life-critical task. This marks a fundamentally different approach from broad, surface-level solutions. The Russian development demonstrates that the future of medical AI lies not in universal models, but in precise algorithms tailored to specific diseases and trained on high-quality, verified national datasets. This approach opens the door to an entire ecosystem of digital diagnostic assistants.

Resetting the Healthcare System
The importance of this technology for Russia is difficult to overstate. Deploying such systems could reshape the healthcare landscape, particularly in regions facing shortages of highly qualified pathologists. A digital pathologist acts as a force multiplier, enabling specialists at major medical centers to work more efficiently while giving physicians in remote hospitals access to expert-level decision support.
Following the completion of clinical trials in 2026 and the start of pilot use at leading medical centers, the path toward large-scale integration will open. By 2027–2028, after registration as a certified medical device, the system could become a standard component of laboratory information systems nationwide. This would lead to a systemic improvement in early gastric cancer detection, lower mortality rates, and reduced pressure on costly high-tech oncology care. Investment in prevention and early detection is consistently more cost-effective than treating advanced-stage disease.